Dr. Anna María Pálsdóttir is the Senior Lecturer/Assistant Professor in Environmental Psychology at the Swedish University of Agricultural Sciences (SLU), the Department of People and Society. She is a professional horticulturist with a BSc in Biology & Horticulture Sciences and a MSc and PhD in Landscape Planning and Environmental Psychology.

Dr. Pálsdóttir works with conceptual development and scientific evaluations of nature-based and nature-assisted interventions that are conducted to various outdoor environments for different target groups. Her research also focuses on the content and design of sustainable outdoor environments for human health and well-being. The research is conducted in close collaboration with national and international universities, governmental offices, and various stakeholders.
Additionally, Dr. Pálsdóttir has a vast graduate level teaching experience. She is one of the founders of the Outdoor Environments for the Health and Well-being Master’s program (OWH) and has developed many courses focusing on nature-based and animal assisted interventions and sensory expression in outdoor environments. She is one of three SLU educators running the SLU Landscape Teachers Synergy Forum.
On the 4th of July, 2024, I sat down with Dr. Anna María Pálsdóttir in a cozy office with a view towards an oak forest at the campus of the Swedish University of Agricultural Sciences (SLU). We had just completed a round of field trips to the locations of the Nature-based Rehabilitation (NBR) program providers, also known as the Skåne-model, or Naturunderstödd Rehabilitering (NUR), which she facilitates as the academic advisor.
The program is founded on extensive research from the Alnarp Rehabilitation Garden, run by SLU. It emphasizes the role of nature in aiding patients to recover from stress-related mental illnesses, specifically exhaustion syndrome, mild to moderate depression, and anxiety. You can learn more about the program on this blog post.
In this interview, we discuss Dr. Anna María Pálsdóttir journey into the world of academic research, specifically on nature-based solutions , and the origins of the NBR program. You can find the full video format of the interview on the link here.
Transcript:
Annetta: Anna-Maria, thank you so much for sitting down with me. I would like to start the interview by asking, can you tell me a little bit about yourself and how you came to be interested in nature and mental health?
Dr. Anna María Pálsdóttir: I am a researcher at the Swedish University of Agriculture Science. I’ve been interested in nature my entire life, but it wasn’t until I started to do my PhD, or just prior to the PhD, that I understood the importance for mental health by observing what’s around me. Also through my previous work in Iceland in the botanical garden, and seeing how people came not only for learning about plants, but for pleasure and wellness. And that led me towards focusing on plants and the environment, the landscape, and into more environmental psychology and public health. Thinking about how we can build and use nature and natural elements to promote our health.
Annetta: Can you discuss some of the work that you’ve been doing within your research that directly connect with mental health and nature?

Anna María Pálsdóttir: All my work has to do with this interaction of environment, the outdoor setting, where the natural environment and natural elements dominate, and how different people connect and use nature. We as a research team look specifically into the qualities and properties, and the sensory stimuli from the natural environment and how we can promote health both in everyday life and also in specifically rehabilitation settings.
Then we have a long-standing collaboration with the healthcare authorities in Skåne, our county, to find a way to use nature to be part of the healthcare system, which is now implemented, and how we can get nature to be a regular part of our public healthcare. We are celebrating 10 years this year since the first implementation, but we are always leveling up for every procurement there is.
And we have been through three procurements. We level up each round using evidence-based methods. We look into all research, medical, healthcare, landscaping, and environmental psychology and find the best reasoning and motivation behind them. And now we are also heading towards doing an evaluation of this 10-year project to see the health effects, the reasons behind why the healthcare authority or primary healthcare professional refer their clients. Are the patients happy? What’s their experience? And, of course, for those running nature-based intervention provider centres, what are the pros and cons, and what do they need?
We talk a lot about sustainable business management and sustainable management of the outdoor setting and sustainable health. It’s all linked. And we’re going to look into all those aspects and try to to understand, to describe and build in more evidence if this is working as a health-promoting tool.
Annetta: Before we dive deeper into the program you’re running now, I want to discuss the context of the Swedish healthcare system. What were the things you were seeing before you started your work within the healthcare system? And what were the needs that you thought you could help in developing and improving?
Anna María Pálsdóttir: Well, actually, the help and the reach-out came from the healthcare authorities.

The research team here in Alnarp, run by Professor Patrik Grahn, was looking for a way to collaborate with the healthcare authorities and they did with a good result. [The healthcare authorities] realized that this is something to be counted on in the healthcare system to be implemented and something that could be used and beneficial for illnesses that are lifestyle-related.
You cannot just give a cure pill or treatment for something that has to do with lifestyle and working situations. And so, this reach-out came from the healthcare authorities saying we need more alternatives. They said they see that this is really working, and could they collaborate and find a model we could implement. So, that’s actually how it started for me to be part of that team.
Annetta: Let’s say somebody who sees a need in their own country, what would you suggest to them if a country does not have this kind of reaching-out system but does have a need that would have been similar to Sweden’s need?
Anna María Pálsdóttir: I think it’s reasoning and showing best practices, having a dialogue about what are the challenges. There are always similar challenges somewhere else. Could this [approach] be implemented? So, it all starts with dialogue. And starting to have a mutual interest and wanting to find a solution.
Annetta: Now, let’s dive into your program. Can you take me through it step by step? Let’s say you came into the meeting with the healthcare authorities. How did you go from Step A to actually implementing this program and who are the different actors?
Anna María Pálsdóttir: Well, it takes some time and you’re not doing it alone. You’re doing it as a team. We have a team from the university. We have a team from the healthcare authorities in Skåne. We have the social security system and we have the labor market representative for all of those because everybody is coming and has connections with somebody who is on a sick leave. We came together and started not exactly from scratch. We had experience from a rehabilitation garden project we ran with the university.
So, it starts basically with mind mapping. Who has what responsibility? Who can do what? And then gradually build up a feasibility study. We did a two-year feasibility study before this was implemented and pulled data and research from different sites as well. So, it’s kind of the multi-steps starting from quite simple to quite complicated. But it doesn’t end when you implement [the program].
You need to follow it through and see that the quality remain the same throughout. Not the same, of course, for the quality needs to improve in all aspects. So, there are many steps. It takes time, but you have to be committed and believe that there’s a solution always ahead and reach those solutions as well and then go on to the next step.
Annetta: Did you see any resistance from any of the actors in the beginning stages?
Anna María Pálsdóttir: Not really. We had committed champions from the different governmental offices. They were keen on exploring how can we solve this. But within each kind of system there is always a skeptical mind. And then you just need to understand what kind of information you need to share with them. Also starting a dialogue and having understanding communication, not just throwing evidence on people, but also understanding what are the needs, why do they want to know more, what they don’t want.

Maybe they don’t want to know more and they’re just ignoring it. Fine. But, of course, you will always have the voice that is says there’s not enough evidence. “We need more evidence!”
Of course, we do. That’s where research comes in. Otherwise, I would be out of work. We have to think that today this is our knowledge level, but we can always level up. But we can also say we know a lot already. We have a lot of research backing up why nature is good for you, why daylight is good for you, why exercise outdoors is good for you. Combining this into health care, this is not rocket science. I think it’s a really good point that we have a lot of professionals working within the health care system that want to move outdoors. They are trained indoors, but they see the benefits of bringing their clients outdoors.
We can talk about two kinds of rooms, indoor and outdoor. Those professionals want to come out because they see the benefits. Many have said that I can help my client in a much better way when we are outdoors with all the sensory stimuli than indoors. I think within this system where there are critics, they are slowly understanding that this is really not rocket science. It’s basic human things. We are born and raised in nature. We come from nature. We did not being born in this kind of environment. Coming out and getting back into, as I said, daylight, multi-stimuli.
We have more physical possibilities and physical activities. Even when we are indoors, we have created a scene and people take their role and position. I’m a teacher. I have my students in front of me. But when I’m outdoors with them, everybody has knowledge to share. Everybody is an expert on something. That kind of becomes a much more dynamic learning environment. So I see this as a teacher. And I can definitely imagine those who have got the taste of it, bringing your clients outdoors, how much valuable it is. I’m not saying the one thing is better than the other, but we should see the equal possibility to be indoors or outdoors. So you have your program.
Annetta: Can you tell me the name of the program?
Anna María Pálsdóttir: This particular program is called Naturunderstöd Rehabilitering på landsbygden, region Skåne modellen. So basically we call it NUR Landsbygd Skåne modell. And it is implemented through, in English, a kind of nature-based rehabilitation in the countryside, and it’s called Skåne model.
Annetta: Can you tell me who this program is targeted for and the elements that built this program into what it is?
Anna María Pálsdóttir: It is targeted for individuals or you could say a “patient” clinically diagnosed with mental exhaustion or burnout, depression and anxiety. This is like the primary target group. So if you have one of those three, you have succeeded with the inclusion criteria. So it’s particularly done for those three clinical diagnosis. And this is not a treatment. It is an add-on to ongoing treatment as a support.

This is giving the clients or participants them the possibilities to mental recovery and physical recovery in an undemanding environment. And, as we said, being in daylight, because many of them are indoor all day, never going out, not even to shop or meet family. So just coming out, breaking the social isolation, meeting other people in the same situation seems to be also very important because you don’t have to explain yourself. Everybody understands. In that sense, it’s a freedom.
You can just do what you need. Basically, a lot of people that start with rest in nature, we call it you are resting in, you’re awake but you’re resting. And those we have interviewed say, this is not the same rest as being indoor, sitting on your couch. Here you have a moderate stimuli of smell, what you hear, natural sounds, what you see. And all of those things are kind of helping you to calm down. Then gradually you build up your energy.
Many have said that after a while, when they kind of recover, they say that it’s like they were on their knees but now they’re standing up. This is the comparison they’re using. Then they can start to use more rehab alternatives because when you have, for example, mental exhaustion, your executive function are out. So the cognitive side of thinking and making sense of things is not there. And this is also about how to get down into the body, feeling alive and one with your body. Some people don’t even smell anything. They don’t really feel anything. So it’s about getting back to your body and gradually coming up in the thoughts and being able to make sense of what’s being done in the other rehab alternatives.
Annetta: How do these patients or clients able to get into the program?
Anna María Pálsdóttir: They are referred by primary care. The medical doctor makes the diagnosis and if they fit one of the three criteria, the “primary criteria,” you can, if you want to, be referred to this intervention.
Annetta: And what is the “primary criteria”?
Anna María Pálsdóttir: You have to be diagnosed with one of the three ICDS codes: mental exhaustion, depression, and anxiety.
Annetta: Can you tell me a little bit about the providers?
Anna María Pálsdóttir: If you’re diagnosed with one of these primary criteria, I [as the medical professional] would say, okay, there is the list. You take the list and say, okay, who’s offering this? Where do they live? You’re allowed to go anywhere. So you could find their description, what they offer, where they are. And then you could say, ah, this one is really interesting. You make contact and say, I would be interested to come for a visit just to see what your place is about. You visit and feel comfortable with them. You may think the environment is interesting.
Or maybe you’re into horses. There’s a horse there, so you want to stay. So then you decide you’re starting. Then the primary healthcare will send a referral through the healthcare system and say, Ana Maria is coming and she’s chosen that particular Nature-based provider, NBI provider. And then you can start your eight-week visit. But you don’t sleep over.
Annetta: They just come for half the day. Is that correct?
Anna María Pálsdóttir: Four hours a day, three days a week. And you need to be able to manage this trip back and forth on your own to be able to be part of the program.
Annetta: How do providers become providers? What is the process?
Anna María Pálsdóttir: Through the official procurement. That means there is a list of all kinds of things you have to pass, basically. There’s a legal issue, there’s a business issue. Then it comes to your outdoor environment, and it comes to the program and who’s working there and so on, what kind of profession do they have. So, there is like a list of qualifications.
If you pass that, then you’re in the evaluation. So, this is kind of first sorting out yes and no. And when you get the yes, you will go into the stage of a more detailed evaluation further on, especially about the outdoor environment and the program.
Annetta: What do these providers and their locations look like? What are these certain criteria that they have to tick off in order to be able to qualify?
Anna María Pálsdóttir: Actually, many. There is everything from the physical properties, what’s there, what kind of greenery or plants and landscape there is, also how it’s connected with each other. There is like quite a long list you need to tick for the environment, for other facilities that you need to be able to access, and also accessibility. You need to be able to get there.
So from our experience, if you’re too far out, or it’s difficult to get there, you will not get the clients. You need to also think about the placement of where in the county you are and how easy it is to access your place. A lot of these providers, they obviously have work themselves, they have other business that they run.
Annetta: So what is the pull for these people to become providers? What are your thoughts about why these people running these places want to be with this program?
Anna María Pálsdóttir: I would say, I haven’t done any evaluation, but my experience and take home after 10 years working closely with providers, is that they are interested in people, they are interested in nature, animals, and they are interested in welfare in general. There are, of course, people that are business-minded and are doing it for more financial gain, but there is always a heart. There is always a heart in there.
I have not met anyone without the heart, kindness and care for both the environment and people. I think that’s the general profile of a provider.
Annetta: Walk me through a day of a client at one of the providers.
Anna María Pálsdóttir: Everybody has to follow a certain structure, and that structure is based on our research. What our client said was they wanted a safe environment where they felt secure and safe.

The start of the day is the welcome. You gather the group and you see who’s here. The welcome is quite short, or it can be short, but then you move on to the patient’s own time. They find their spot, they can walk, they can sit, they can do whatever, but it’s their own time to relax and come even further down to the relaxation. Then there is an open offer and an invitation if they want to be part of some activities, and they can choose if they want to. And if they aren’t up to it today or they have the urge to walk or an urge to sit in the sun or whatever, they can do that. But there is also an organized activity that they are invited to participate in.
That’s really important. The participants themselves are not running the project. They are like guests and they can go in and out as they please, without any explanation. So they could come and look at what you’re doing, and then realize they don’t really want to do this.
They just withdraw without having to excuse themselves or explain anything. This is something we learned from our research that it’s really important to be able to have the freedom here, because quite a lot of people in this situation are used to making sure everybody else is okay and never attending to themselves. And now this is the time when they can attend to themselves and their own needs.
Annetta: How would you define success of the program? Or how would you define success for each participant or client? Have you had any feedback or gathered any data?
Anna María Pálsdóttir: Yeah, definitely. Especially from the research we did two years prior to this implementation. We saw that there is this way, they call it, I come back to myself, I can feel I’m alive, and I feel I want something. You could call it an awakening. Coming back to life is one of the successes. That’s actually the basically first step of moving forward, not to be in the same place as always. Even though the entire program and the research is based on people that have been on sick leave for a shorter time, we have clients that have been on a sick leave for 3, 5, 7, 8, 9 years! That’s a quite long time.
Of course they are helped by the program, but this should come much earlier in their sick leave to be helped back on track. They have a new orientation, they rediscover an old interest or they gain a new interest. It’s really kind of seeing hope, seeing the light, and wanting to go on, not being just sick and giving up. Many have just given up on everything. Even on their family and friends. So, coming into our environment where you can feel normal, you can actually laugh, and you can feel happy, that is kind of setting the process of, we could say, happy hormone. And of course you do sport or something else, that’s also how you level up your happy hormones.
This is one way to come in action again. What we see of course is also that in the pilot and the feasibility study we did before, we could see that every person in that program over two years, moved from being more or less on a sick leave to starting to move forward 25%, some 50%. They were moving forward toward, you could say, the labour market again. But it has to become an option much sooner when you’re on sick leave.
Annetta: How do you continuously evaluate and ensure that the program is running to high quality standards? You mentioned the procurement coming up. What is your process and what are you doing now?
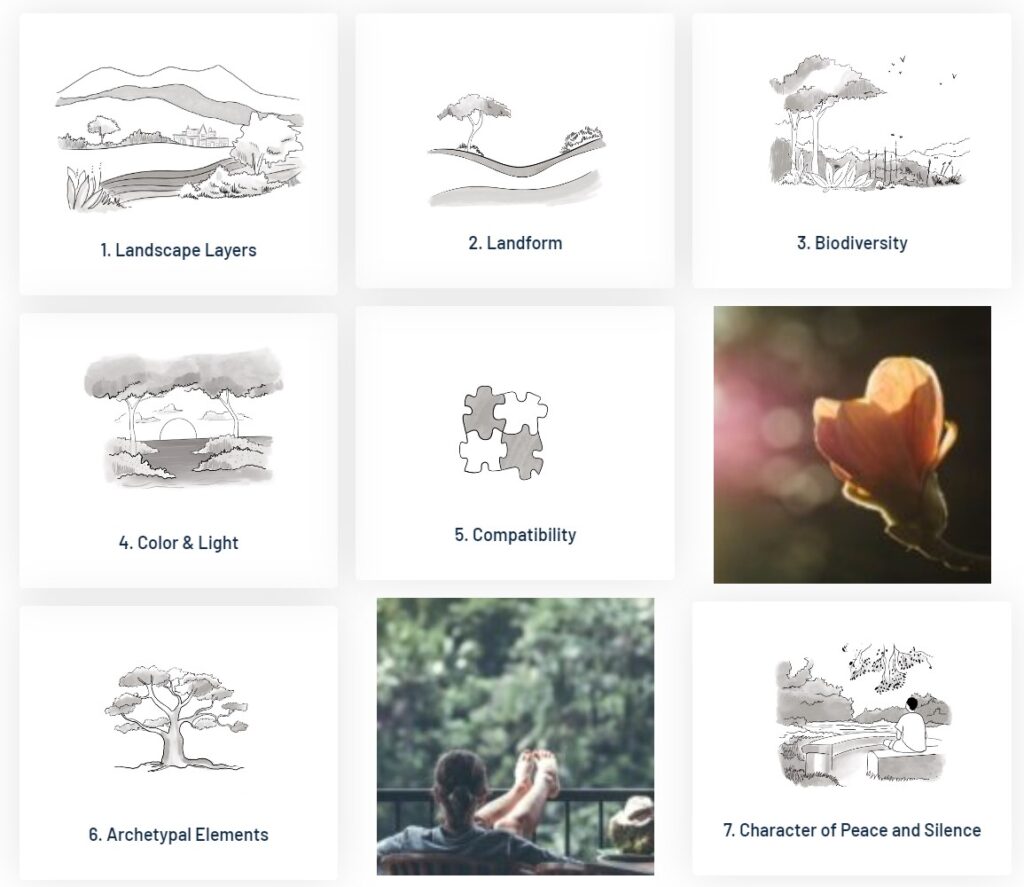
Anna María Pálsdóttir: I have been looking for more methods than we have implemented. How can we ensure that the outer environment we are selecting actually hold high quality and are actually restorative? And yeah, we stumbled on a very interesting model, the Contemplative Landscape Model, that is research-based, which is really what it’s about for this group of clients. They need this kind of restoration.
We have just tested the CLM in the field to see if we can use this kind of method to evaluate the places. And yeah, definitely we can. So, now the next step is to put it into a more concrete way of how we would do it in the procurement.
Annetta: Tell me about your first time trying the Contemplative Landscape Model out in the field.
Anna María Pálsdóttir: It was fun! What I learnt was that there were qualities in the landscapes [of our providers] that were there but I was not paying attention to them. And we were really focused on the [providers] closest to nature or the environment. And in this model, we also realized how important this outer space or outer zones were.
Anna María Pálsdóttir: It was fun! What I learnt was that there were qualities in the landscapes [of our providers] that were there but I was not paying attention to them. And we were really focused on the [providers] closest to nature or the environment.

And in this model, we also realized how important this outer space or outer zones were. That would be very hard to place these kind of providers in the urban setting because you would not have those qualities there. I suspected that we were in the right spot out here in the countryside. But now we have the proof.
Now we’re studying forests as a healing environment and we want to investigate if we can apply the CLM method in that context? Does it have to be modified in any way? The base is there and there are a lot of things we can already take. It will be very interesting to apply it to a forest landscape. Where do we find the restorative potentials? We have a lot of data from clients in different parts of Sweden where they talk about which qualities are important in forest bathing and forest therapy.
We will start a larger study and then we will pull out those details and see, can we actually confirm them by this framework? Yes we can. We’re very excited to see the CLM coming to Sweden. The reason for it coming to Sweden and being propagated here is because of [NeuroLandscape and especially its founder and director, Agnieszka Guizzo. So, you know, we’re very, very grateful for you being such a force behind the method.
Annetta: Why do you think Sweden is such a powerhouse in adopting the CLM into its national healthcare protocol? Besides you being the superwoman pushing nature-based solutions forward? Sweden is the first European country to kind of adopt the CLM into its public healthcare system. Singapore is the first country in the world.
Anna María Pálsdóttir: I think it’s because we have people around us that are interested in development and so have a better-quality output in the service they provide. And they want to offer the service with other alternatives, not just one. So this is one nature-based out of many.
I think if you look at Sweden as a whole, the county of Skåne is the first to implement this in 10 years and three procurements and hopefully the fourth. And that’s just showing that maybe in this region, there is a force of people that are interested in service development, innovation. They are front runners and forward thinkers. I wouldn’t be able to do any of this if it weren’t for colleagues and collaborators within the healthcare system. I couldn’t.
So you could say this is co-creation. It’s a buzzword but this is real co-creation where we come in with all our knowledge. One thing I feel also in this collaboration is this respect for each other’s competence. And I think that’s also one of the primary factors why we’re moving forward. And it’s not enough [for the program] to be implemented. We want to do more. And we do it as a team.
The team from the healthcare authority have come out to meet the providers. They really show an interest. That’s really important for the providers because then they realize this is serious business. It’s not just open up the garden or the forest or whatever — it’s really serious business. And that makes them also more serious in their work to provide a high quality service.
Annetta: So, what is your main goal then? What would you like to see being achieved in the Swedish population or within your community? What would make you sit back on your couch and think, yes, we did it.
Anna María Pálsdóttir: I don’t think I could sit on the couch. I think I would always be like, what’s next? Maybe I would take rest in the garden or the forest…I would say success is feeling accomplishment. I feel we have accomplished a lot, but I think there is this mentality of wanting to do better tomorrow than we did today and do it in a manner that is also evidence-based. Also, the courage of saying, “Let’s explore what is not really known.” That’s actually the way forward, not just to stay there. There’s always something you can do better.
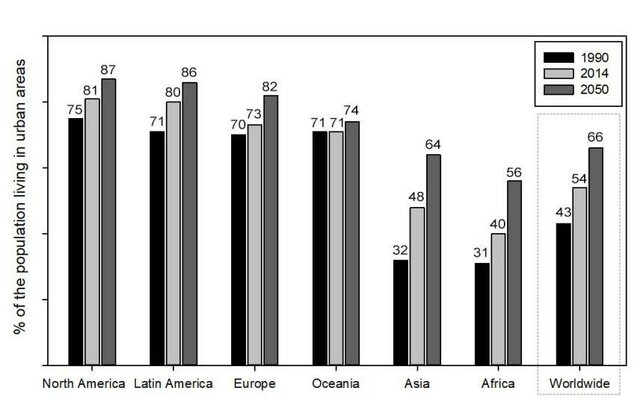
I would like to see this kind of program implemented for the entire society. That we have more than nature and greenery in our everyday life. I would like to see this in the kindergartens, schools, elderly homes, hospitals. We should be bringing more nature into our everyday life.
Perhaps there will be less need of rehabilitation because we would have this more health-promoting environment in everyday life. Also, I would like to see those who work in health care and are treating people have the possibility to take the clients outdoors. This should also be implemented in the architecture because quite often when you’re designing, you design the building and there’s a lot of focus on the indoor. And then there’s the outdoors and it’s on its own. [The two] should be merged so you would see [the indoors and outdoors] as one, as one whole. When you design, for example, a hospital, you’re thinking in both ways. That there’s an outer room and an inter room. And as a professional, you should be offering both. I would like to see that happening as a general rule.
Annetta: We’ve come to the end of our interview. Are there any last thoughts that you’d like to share?
Anna María Pálsdóttir: Well, I would say I’m really happy that [the NeuroLandscape team] came. I’m really happy that you shared your knowledge and experience. I think this has really pushed forward our work and arguments showing how our way of evaluating the outer environment can be improved. And this can be used in so many other aspects, not just for the procurement.
But I would like to see this as well introduced to our students because then they can take it out when they graduate and start to work in different places in the society. They can have this with them because I think this is the way forward of understanding the science behind the framework.
We need to be able to open up and share and respect each other’s role, leveling up and k finding ways of collaborating, growing and developing. So we get together and then we make something out of it. Like a flower.
Annetta: We are very grateful for the invitation and we’ve had a lovely time. Thank you.